Sexual Health (young people)
The contraceptive implant
There are four methods of long-acting reversible contraception (LARC) to choose from; contraceptive injection, the contraceptive implant, the intrauterine device (IUD or non hormonal coil) and the intrauterine system (IUS or hormonal coil). This page is about contraceptive implants.
LARCs are known as “fit and forget” methods; this means once they are fitted or given, women are protected from getting pregnant until it needs replacing.
“If implanted correctly, it's more than 99% effective. Fewer than one woman in 1,000 who have the implant as contraception for three years will get pregnant.” (NHS Choices)
The contraceptive implant has the lowest failure rate of all methods, this means it is the most reliable, and the fewest women get pregnant whilst using it.
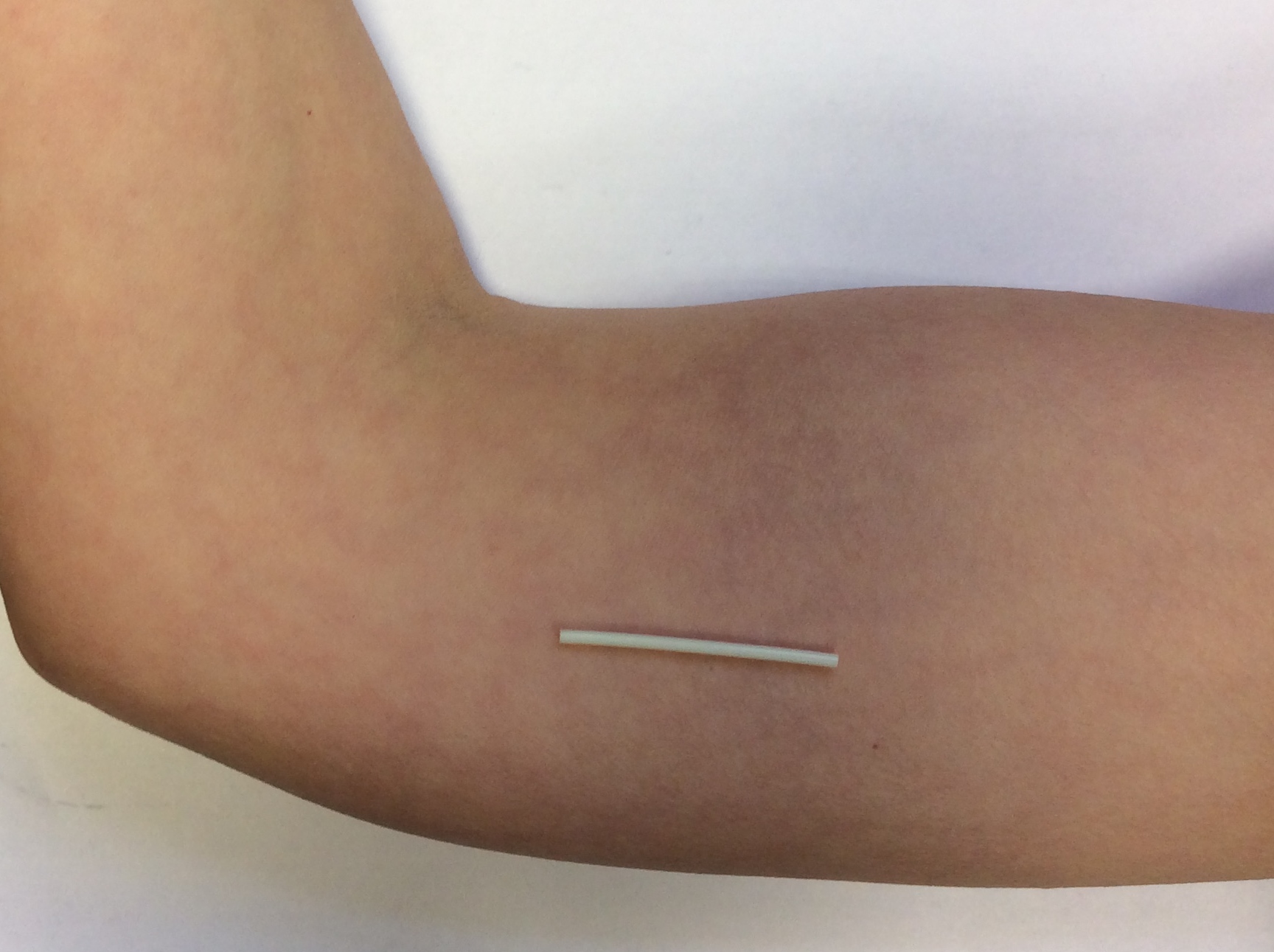
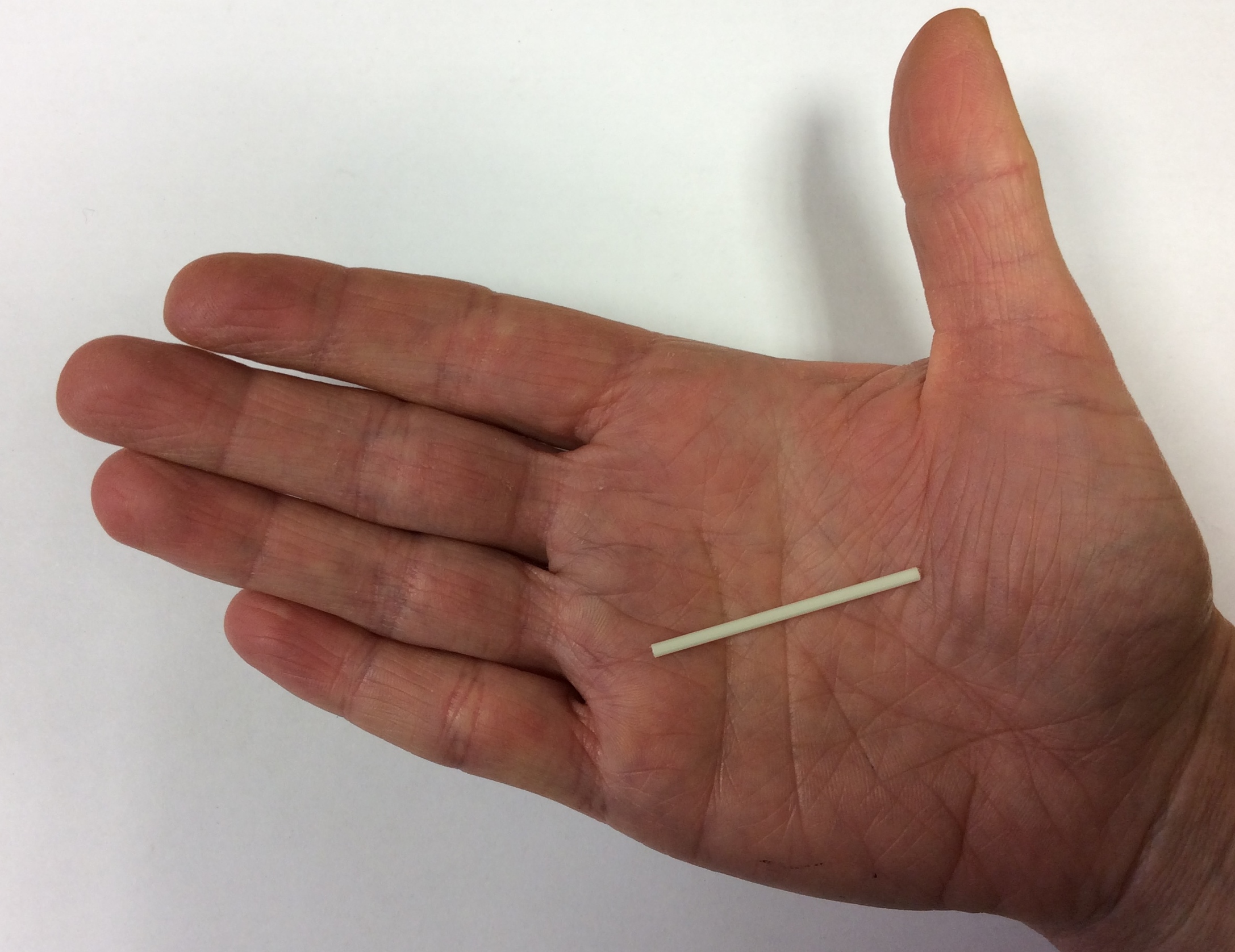
A contraceptive implant is a small, flexible rod (the size of a match stick) that is put in the upper part of the arm and works for up to 3 years. The implant contains progesterone. This stops ovulation (releasing an egg every month), thickens the mucus in the cervix (stopping sperm reaching an egg) and also thins the womb lining.
Size of the contraceptive implant
Position of the contraceptive implant
It can be removed at any time if it doesn't suit you, but doctors recommend it is tried for three to six months before making a decision to remove it.
Natasha talks about the consultation with her GP where she learnt that high blood pressure and being overweight can prevent women from having the implant.
Natasha talks about the consultation with her GP where she learnt that high blood pressure and being overweight can prevent women from having the implant.
So I made an appointment with my university GP and I went in and I said, ‘I would like to get the implant’. And when I did it the implant was still new so they were still really, really excited to be able to have willing participants saying, ‘I want the implant’. And I went in and you have a consultation and they show you how it will look. They give you, I don’t know, some kind of mock up of a human arm because that is where it will go. I don’t know if you can see it on camera but can you, do you want me to show that it goes in there? Just so people can see what because this is where it will go for everyone.
Victoria was told that she could have the implant removed if she wasn't happy about it.
Victoria was told that she could have the implant removed if she wasn't happy about it.
You have the option to go back. If you've got any concerns, you have the option to go back even within a month and get it removed if you don't like it. It's completely up to you and any woman who says, "Oh they wouldn't take it away from me," and like, "My doctor said keep going for three months and I didn't want to." She obviously didn't go on the internet and type in Family Planning clinic in my city because it's not hard. My doctor was rubbish, gave me no information and when I contacted the reception to see when I could make the appointment she offered me one in about three months' time which I didn't want, I wanted it sooner than that. So my doctor was absolute rubbish which is why I went to my local GUM clinic. And there were two others attached to the university hospital that I could have gone to but I went to the Family Planning one just because it was closer. Three in one city and, you know, it's not a big city because I was in [city], three but you know so if you're living anywhere that doesn't have one you're probably in a village in the middle of nowhere. It's impossible to not have it done and if someone tells you they can't take it out, go somewhere else because you're entitled to have it taken out if you don't want it.
You were told that?
Yes. You don't have, they recommend that you keep it in for three months because after that the side effects will stop and you'll probably like it but if you don't want it for the three months or you put it in and suddenly you've gone up half a stone already and you're bleeding all the time, you're very welcome to have it taken out and go back on the pill or go on to condoms or go on to any other thing you want but it's your choice and it is always your choice and that's what they stressed to me which is why they were so different from my doctors. Your choice, if you want it you have it, if you don't come, we'll take it out.
One of the main advantages of implants is that women don't have to worry about remembering to take anything, so they are good method for people who are a bit forgetful. It is important to remember that the LARCs do not offer any protection against sexually transmitted infections. If there is any possibility of infection, condoms should be used as well.
There can be many reasons for a woman to change the type of contraception they use; concerns about the side effects of the pill, wanting to stop using condoms, having trouble remembering to take the pill, concerns about the effectiveness of the pill when sick, irregular or painful periods and bleeding or to reduce the risk of pregnancy. People may also want to change because they have had problems with other methods of contraception.
Life has a student can be hectic and that's why Hannah has been advised to consider having an implant rather than using the pill, but information about it can be confusing.
Life has a student can be hectic and that's why Hannah has been advised to consider having an implant rather than using the pill, but information about it can be confusing.
Sometimes I’m a little forgetful and a few times I have forgotten to take it which I get very annoyed at. So I’m thinking of switching from the combined pills simply because it’s. I want something that I don’t have to remember to take every day, something that I don’t have to think about every day.
Hannah knows that if she is drunk and then sick, the effectiveness of the pill is reduced and she may get pregnant.
Hannah knows that if she is drunk and then sick, the effectiveness of the pill is reduced and she may get pregnant.
Well I know that when I drink alcohol and as a university student I drink a lot of alcohol and I know that when I go out and when I do drink and get drunk I will get forgetful and I will forget to take my pill if I took my pill in the evenings because I try and take them at the same time every day. And if I take my pill in the evenings and then I go out and get drunk what often happens is that I’ll get very drunk and I’ll end up being sick. And then I don’t think if it happens quick enough I was told that I wouldn’t have time to absorb the pill. So it would be as if I hadn’t taken it at all. So this was, this was a major concern of mine just in terms of if I drink alcohol and I do get sick will the pill still work but if it’s not fully in my system.
Avoiding an unwanted pregnancy is Hannah's main priority but she has concerns about how effective the implant is, and about the prospect of using a method that stops periods.
Avoiding an unwanted pregnancy is Hannah's main priority but she has concerns about how effective the implant is, and about the prospect of using a method that stops periods.
I’m still not quite sure what I want to do.
The implant commonly changes a woman’s bleeding pattern, including stopping periods altogether. The bleeding pattern is not an indication of whether the implant is working – whatever the bleeding pattern they are extremely effective at preventing pregnancy.
Some of the women interviewed chose to use implants as their method of contraception after trying the pill or condoms.
Describes how she realised she needed a more reliable method of contraception and discusses the role of her GP in providing advice. (Actor)
Describes how she realised she needed a more reliable method of contraception and discusses the role of her GP in providing advice. (Actor)
(The accompanying video and audio clips are played by an actor)
You were sort of not using condoms or anything?
No I wasn't. I just had unprotected sex every now and again but it was with the same guy because I was still with him, but then we got a bit worried and I'm thinking oh no, what if I fall pregnant, what am I gonna do then. So that's when I went to the doctor and said 'Look seriously I need something.'
Because I kept on going for the morning after pill. Most of the time I went for the morning after pill and they'd say "the morning after pill's not really good, you're not supposed to really take it more than three times in a year", and I did take it more than three times in a year, you know what I mean' Yeah seriously, I did.
That's when they said to me you know 'You seriously need to think about long term, contraception'. So then yeah that's when Depo came in to it. Because like my GP, I've known her for a long time and she's been my childhood GP, she knew when I left home and everything so she knew she has to be there as an extra support for me as well to explain everything to me.
And then obviously you go to see the nurse for contraception and things like that, so she transferred me to a nurse who explained all the procedure to me.
So like if I had a problem the first person I would go and see would be my GP because I can really, really trust her, she's like a friend to me, someone I can really openly talk to, so that's nice.
Describes how she decided to have an implant. (Actor)
Describes how she decided to have an implant. (Actor)
(The accompanying video and audio clips are played by an actor)
Because first, before I never thought about implant, and when, when I knew it was working and everything I found it really marvellous. I was like, wow, for three years, and you don't even need to take the pill every day to remember it, and this kind of details.
But it makes it better. And now it was nice, I felt nice when I read the prospectus about it, I found it really nice, so I thought, I'm gonna start to study next year, I'm not planning to have children the next three years and anyway, if I change my mind I can take it out.
My metabolism will come back normal as soon as you take it off, contrary to the pill that, it takes time for the ovaries to work properly and everything. So, I don't know, I found it more safe somewhere, like for your body and everything, so I decide to change. Maybe in three months I will complain and I will say that it was a really bad idea, but I want to see...
Before changing contraception methods there are leaflets to read about what's available or health professionals to talk to at GP surgeries, Family Planning or Brook clinics. Implants don't suit everyone so it's important to get information to help make the decision.
Women we spoke to had different experiences of contraceptive implants. Women often reported being happy with the implant but some had stopped using it because of health concerns. Some others used implants or injections as contraception after childbirth.
Victoria explains why she is happy using the contraceptive implant. She plans to use it long term.
Victoria explains why she is happy using the contraceptive implant. She plans to use it long term.
For Natasha, the contraceptive implant worked well for two months but then she started to experience irregular bleeding for almost a year. She had it removed.
For Natasha, the contraceptive implant worked well for two months but then she started to experience irregular bleeding for almost a year. She had it removed.
And for the first couple of months it was great. It was fine but then it all started to go really, really iffy. I had a lot of breakthrough bleeding and I think, I think nearly for about two months it was like I had a period for two months. So I had two months without anything then two months with it, two weeks without, another four weeks with it. So completely ruined my entire cycle, just completely ruined it. And because I think the thing you have to remember is when you get these things put into your body they are releasing a chemical hormone into you that your body may naturally produce on a small scale but when you put it [the implant] in that amount is going to have an adverse effect on your body and the balance and everything which I think you get told but I don’t think you get told it in enough detail like.
But I found that doctors are very much, these are your options. Pick one that you think you kind of like and see how it goes. They don’t really warn you that when you put this into your body you are essentially messing yourself. You are messing up your cycle because after, I’ll get onto it, but after I took it out it took about six months for my cycle to go back to normal which, you know, it’s not very convenient really because you can’t really do anything because you don’t want to put more chemicals in after you’ve just taken chemicals out. And so that went on. So I had it in for about, I think, nearly a year before I was like, ‘No it has to stop. I’ve given it a fair shot and I don’t want to be dealing with this anymore.
So I went to my GP. I told them what was going on and they said, ‘Ok fine it sounds like you need to have it taken out’. And it’s, it was ok. I made an appointment. Went in, completely at my own, what’s the word, at my own convenience and I went to surgery and it was a really weird procedure. You lie down and of course they put in the anaesthetic again and they slowly slide it out and you can kind of. You don’t really want to see it when they slide it out because you know what it looked like going in. And yeah they took it out and there, and yeah. And it took a long time for it to heal up and like I said it took six months for me to, for my body to go back to normal.
Irregular bleeding is a common side effect of the implant but it doesn't mean it's not working. If this happens it is worth talking to a doctor or nurse for advice. Sometimes taking a contraceptive tablet as well as the implant can settle the bleeding down. Because the implant provides contraception, forgetting to take the pill doesn't result is an increased chance of getting pregnant.
We talked to women who had stopped using LARC and are now using other methods, such as one of the contraceptive pills. Many said that they find it difficult to remember taking it every day. Stefanie reminds herself with an alarm on her mobile and by keeping the pills next to her toothbrush.
Reasons for not using LARCs or stopping using them included: the experiences of relatives or friends, ‘horror’ stories reported by the media, concerns about LARCs' impact on fertility, and the feeling of losing control over their own bodies.
Sarah didn't consider the implant as a contraceptive option because she dislikes the idea of having it under her skin. Besides, her GP didn't say that it is a reversible form of contraception.
Sarah didn't consider the implant as a contraceptive option because she dislikes the idea of having it under her skin. Besides, her GP didn't say that it is a reversible form of contraception.
Last time I went to my doctors to get my next packet of my pill was in the summer holidays and I was in City so I waited for my actual doctor this time and they said, I just said, “Could I get another packet?” And then he said about getting the implant in my arm and saying how it was more efficient, safer and could have it for three years and it doesn’t mean you have to remember to take a pill every day. But I said that I wasn’t really interested.
Women we interviewed commented that the amount of information they got from their GPs regarding LARCs was variable and that, often, they were given leaflets to read rather than the time to talk about the different options available to them. In towns and cities, overcrowding, lack of appointments or lengthy waiting times sometimes made it difficult for women to access health services for family planning. Victoria thinks that cities offer more choice of where to go for advice than other, less populated areas.
Difficulties in accessing the same clinic for sexual health meant that Stefanie had the implant done in one clinic and the contraceptive pill prescribed in another.
Difficulties in accessing the same clinic for sexual health meant that Stefanie had the implant done in one clinic and the contraceptive pill prescribed in another.
So why did they suggest you use both methods at the same time? What did the doctor say?
The young women we talked to advised others to find out as much as possible before deciding which contraception to use. They also reminded people that everyone reacts differently so not to be persuaded by the experiences of family members or friends.
Natasha advises women to make an informed choice and if in a relationship, to discuss their options with their partner.
Natasha advises women to make an informed choice and if in a relationship, to discuss their options with their partner.
If you decided to become sexually active or if for some reason your doctor said that you need to go on contraception to regulate blood flow or to control your really bad skin or something then ask your doctor for all the potential options. Ask them for all the options that you can have be it the pill, the patch, there’s the injection, the IUD, all of them. Really find out about the options that are available to you because what someone tells you is usually only part of what is out there. And once someone tells you what is out there find out for yourself. Go online because it is completely anonymous. No one is going to know. Find out about these different things. Ask your friends. If you have a sister ask your sister, ask your cousins, you know, but just remember that you’re. I think it’s really hard for girls because you feel like you are alone and you’re not and you’re really, really not because I think there is a certain stigma attached to it if you go on contraception it means, ‘Oh well she is clearly spreading it around isn’t she’. Probably she is not, she’s probably trying to be safe and that is a good thing.
And if you are in a relationship talk to your boyfriend because that’s the person who should be supporting you when you do something like this You know and if you do have a really good stable loving relationship where there is mutual respect and trust have him go to the clinic with you. Have him go through the options with you like saying ‘Well I’m going to get this. Do you feel comfortable with that or would you prefer that I got this or I feel happy with this?’ You know like make it be a really collaborative process about what you are doing because at the end of the day it’s your body but if you are in a relationship with someone, you know.
LARCs are over 99% effective against unwanted pregnancies. But, only condoms or not having sex offers protection against sexually transmitted infections, including HIV.
Last reviewed January 2016
Last updated January 2016
Copyright © 2024 University of Oxford. All rights reserved.