Cervical Screening
Experiences of Cervical Screening
Cervical screening is not a test for cancer. It is a test to check the health of the cervix and to help prevent cervical cancer from developing by detecting abnormal cells.
Cervical screening test (smear test)
Cervical screening is a method of preventing cancer by detecting and treating cervical abnormalities, which, if left untreated, could lead to cancer in the cervix (the neck of the womb). Cervical screening is also known as a smear test.
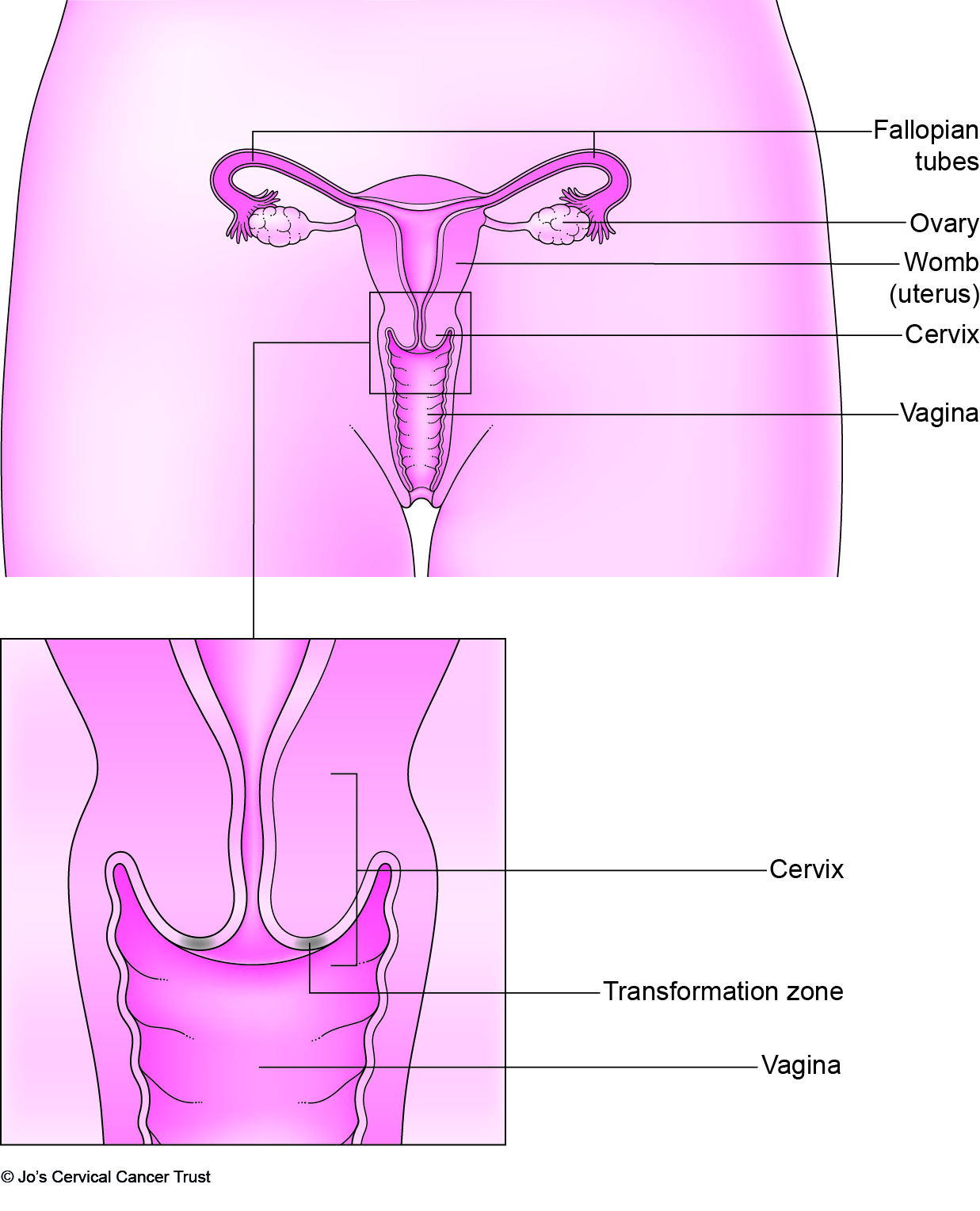
The first stage in cervical screening involves taking a sample of cells from the cervix.
Cervical screening uses a method known as liquid-based cytology (LBC) to test the cells. A doctor or nurse uses a small instrument called a speculum to gently hold open the vagina. A small brush-like device is then used to sweep around the cervix to take a sample of cells (this process is called a cervical sweep).
Once the sweep is done, the head of the brush (where the cells are lodged) is broken off into a small container of preservative fluid or is rinsed directly into the preservative fluid.
The sample is then sent to the laboratory to be examined under a microscope by a specialist scientist (known as a cytologist), who is trained to identify abnormalities in the cells.
For more information see the NHS Cancer Screening Programme ('Resources and Information').
HPV testing
Some types of the Human Papilloma Virus (HPV) can cause abnormal cervical cells. HPV is a very common infection of the cervix.
More than 100 different types of HPV exist (NHS, 27 May 2022); some types are high risk, and some types are low risk for cervical cancer. Around 14 types of HPV are considered high risk for cervical cancer, with the types HPV 16 and HPV 18 being types most responsible for developing cervical cancer (Cancer Research UK, 12 September 2023).
HPV testing is incorporated into the NHS Cervical Screening Programme. Samples from cervical screening are tested for high-risk HPV types that can cause cervical cancer.
If HPV is found in the sample, further testing will be needed. Testing may involve another cervical screening test or a colposcopy (see also ‘The colposcopy examination’).
If HPV is not found, no further testing is needed and an invitation for cervical screening will be sent again in 3-5 years.
For more information about HPV and cervical cancer see the ‘Human papilloma virus (HPV)’ in our ‘Cervical abnormalities: CIN3 and CGIN’ section or ‘Ideas about causes of cervical cancer’ in our ‘Cervical cancer’ section.
Experiences with cervical screening
Some women found cervical screening an easier procedure than others. Many of the women we interviewed considered the procedure to be 'mildly uncomfortable'.
Some felt the procedure was 'an intrusion' or they felt vulnerable, while others found the procedure 'undignified' and 'unpleasant'. Despite these feelings, many said it was important to attend for cervical screening to know that the cervix was healthy (see 'Reasons for attending').
Tina describes her experience of having screening using liquid-based cytology.
Tina describes her experience of having screening using liquid-based cytology.
The nurse told Paula that liquid-based cytology would provide a clearer test result.
The nurse told Paula that liquid-based cytology would provide a clearer test result.
Some women said they made their appointment for cervical screening in the morning after they had showered so that they felt 'fresh and confident'.
One woman said that being provided with a gown helped to 'maintain her modesty' and made her feel more comfortable. Others said that they wore a skirt when they attended for a screening which enabled them to partly cover themselves and to feel less exposed.
Another tried not to think about the procedure too much which helped her to overcome feelings of embarrassment. Some found it helpful to remember that the person taking the test had experience of taking many cervical screening tests and they did not find it embarrassing.
She copes with any embarrassment by realising that doctors and nurses do cervical screening tests all the time.
She copes with any embarrassment by realising that doctors and nurses do cervical screening tests all the time.
Right well to start with obviously it's not a pleasant experience but its something that should be done to save any further problems which could occur. And also I can understand why some women are embarrassed but the way I dealt with it was I just cast aside the embarrassing part of it because at the end of the day these, it's a job to these doctors, they're doing their job and after all it's, it's your health you've got to think of, not so much how the doctor, from the doctor's point of view because I mean it's a job to him, he sees thousands of women and it's just a procedure to him. And without this doctor you're taking a risk really.
There are various information leaflets availoable from the NHS Screening Programme and from other organisations about cervical screening and follow-up (see 'Resources and Information').
Leaflets about cervical screening were available at the surgery and were sometimes given to women by the practice nurse; or, in other cases, were sent to women with the invitation letter for their screening test.
One young woman explained how she felt less anxious than she might have done about having her first screening test because the nurse had given her a leaflet beforehand and explained to her exactly what the test would involve.
Women were often given opportunities during their cervical screening appointment to ask questions about the test. Leaflets are now generally sent with all invitation letters.
Some of the younger women were given an explanation of the test procedure and the instruments used. One woman explained that she found it helpful to be shown the speculum used to open the vagina during the test.
She found it useful to see the speculum used during cervical screening.
She found it useful to see the speculum used during cervical screening.
I remember one of my very first smear tests, I think it was about my second one I hadn't really paid attention the first time round, I was just deeply embarrassed and uncomfortable the first time I had a cervical smear and around the second time I went or the third whoever it was that was giving me the smear test actually showed me the speculum. And I remember looking at it and thinking it's like a double shoe horn or something, it's quite a remarkable piece of instrumentation. And actually seeing it did make a difference for me because I understood really what it was doing. It was opening up the walls so that a proper scraping could be taken and it did actually help to see it and I don't know why they can't make them out of plastic but, but it did help to see.
Some older women had been given explanations about the effect of menopause on hormone levels, and how this can cause dryness and make it more difficult to insert the speculum or cause some bleeding.One woman explained that she was told by the nurse that getting sufficient cervical cells during cervical screening can sometimes be more difficult in women who have gone through menopause.
Sometimes women found it uncomfortable when the speculum was inserted into their vagina. Women who find the procedure painful should tell the nurse or doctor straight away as they may be able to reduce their discomfort.
Tina had no discomfort and did not need to return for a repeat test after liquid-based cytology.
Tina had no discomfort and did not need to return for a repeat test after liquid-based cytology.
Her cervical screening test was uncomfortable but not painful and she believes if you want to be sure you are well you need to have it done.
Her cervical screening test was uncomfortable but not painful and she believes if you want to be sure you are well you need to have it done.
If I could say anything to encourage a woman to go and have their first cervical smear it would be that it would be a compromising situation, put your legs up there and think of something else just for a couple of minutes. It's slightly uncomfortable, there's a metal instrument that is inserted in you, it's merely to keep your vagina open but that it's necessary so that the test can be done. And it's uncomfortable but it doesn't really hurt and so it's just one of those things that if you want to be sure you're well you've just got to do it.
Women who had found it easier to relax were more likely to describe the test as slightly uncomfortable rather than painful. Some found that familiarity with the test, or having children, had made the test less unpleasant.
Many commented that although they had experienced embarrassment or painful screening tests in the past, they considered it very important to attend for cervical screening.
Encourages others not to be put off by painful cervical screening test experiences.
Encourages others not to be put off by painful cervical screening test experiences.
It just I think pulls you up short to say "Well you're, no one is really that safe," and how important whatever your experience of having a smear test done, how important it is to go and have them done and get over that fear, you've got to get over that fear if it's, because you're only going to be worried if it's, supposing one comes back you might have thought to yourself if I'd have gone a year earlier may be that wouldn't have happened to me. So I think whatever the experiences women do need to say, explain the circumstances to your doctor, your clinic, wherever you're going if you've had a bad experience and just be reassured before you have the next one done that they are looking at you when you're telling them and that they're really taking it on board but don't let it stop you going to have one done because it's just not worth it, the worry just is not worth it. I've seen her go through it and it's, and she had regular ones. Nobody is exempt, I realise that but I think my advice to other women who've gone through a bad experience is don't let it put you off because you just don't want to be in a position of a result coming back just because you may have delayed it and you could have stopped it.
Tests are usually performed by a practice nurse, who is usually a woman, but women can also request a female nurse if they would be more comfortable with a female nurse. Although women often said they preferred to have a woman undertake the test, some women had no preference, and a few preferred having a male doctor.
Some said they preferred a doctor rather than a nurse perform the test. Others preferred a nurse because they felt more comfortable, or they didn't have to wait too long for an appointment. One woman who had a previous bad experience preferred to have her screening test undertaken by a doctor or nurse that she trusted.
Cathy prefers having screening with a nurse because she explains what she is doing and makes her feel at ease.
Cathy prefers having screening with a nurse because she explains what she is doing and makes her feel at ease.
While some women wanted to have cervical screening taken by someone that they were familiar with, others felt that too much familiarity would increase their embarrassment.
A practitioner who was more sensitive and provided time for explanation and information was important for many women in their decisions to return a second time for cervical screening.
See also 'Reasons for attending' and 'Reasons for not attending'.
Copyright © 2024 University of Oxford. All rights reserved.



