Systemic Vasculitis
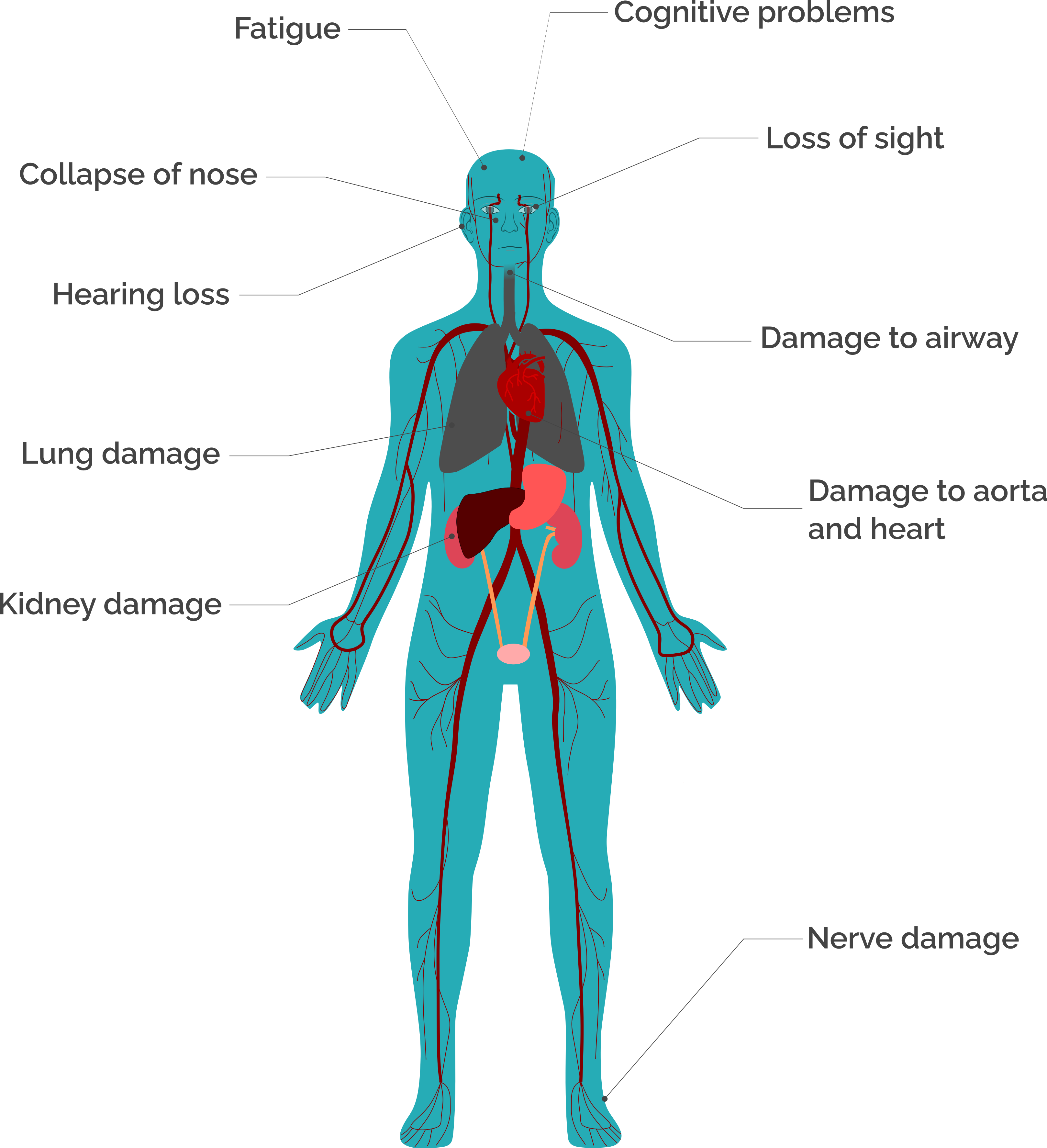
The damage that systemic vasculitis does to the body
- Damage to the body from systemic vasculitis
- Systemic vasculitis and surgical treatments
- Systemic vasculitis and other long-term health conditions
Damage to the body from systemic vasculitis
Vasculitis caused tearing and damage to Diane’s aorta (the main blood vessel coming out of her heart).
Vasculitis caused tearing and damage to Diane’s aorta (the main blood vessel coming out of her heart).
So unbeknown to me, my aorta had dissected at this point, and that’s why I was feeling all the pain in my chest. So, they rushed me to the hospital, the local hospital. They ran some tests and then found out that, yes, there was a problem with the aorta. So, they… at this stage I was very, very unwell and my family were basically told to expect the worst.
They said they were going to transfer me – I was sedated - transfer me to the regional hospital for major, for major heart surgery, but they warned them that the chances of me surviving the ambulance journey was, was 50-50. And then when they got me to the regional facility, the cardiothoracic surgeon came and seen them and said, “Look, I’ll try my best but there’s a very sort of small 20 per cent survival rate for this type of surgery.”
He expected to be in and out in about six or seven hours, but it actually lasted 11 hours. So, when they went in they realised that my ascending aorta from, from the aortic valve right up to the arch, was all diseased and there were ulcers, and the ulcers had formed pinholes, so that’s where the dissection and the regurgitation was coming from. So that’s the amount of pain I was feeling. So, they had to replace the aortic valve, so they replaced that with a mechanical valve, so that meant I was on blood thinners for life. And then they replaced the ascending aorta up to the arch, so they took all that away.
So, at this point, we still didn’t know what, you know, what caused it. So, I was sort of… my main focus was thankfully I survived the operation. They were concerned then, obviously, was there any brain damage, because they were worried, I was maybe unconscious, so without oxygen for a while. But again, thankfully, there doesn’t seem to be an awful lot of damage. I [sighs] am a wee bit more forgetful than I used to be but, and there’s certain things that I can’t really remember, you know, my long-term sort of memory? But apart from that, day to day, it hasn’t really, you know, affected brain function too much.
Losing her hearing was “very frustrating” for Mo but she manages as best she can with hearing aids.
Losing her hearing was “very frustrating” for Mo but she manages as best she can with hearing aids.
Well, yes, but the damage is done, this is the problem. The damage is done, I’ve really looked into that. I mean, I did audios all my days as an occ-health nurse, I knew, I had hearing – no, it’s completely gone in my right ear. All the little hairs that are actually in the inner ear are damaged, they’re never going to come back. Okay? So I hear absolutely nothing in my right ear. But what – I’ve been to actually NHS and it worked for a bit but then it becomes so cumbersome sometimes, the hearing aid. But I went to Boots, and I’m on my second lot, and it did extend to about a thousand pounds a hearing aid, but the technology is quite good. So, I now hear my – when I have my hearing aids in, through Bluetooth, it makes you think and feel that you’re hearing on the right-hand side, when all it’s doing is transferring it via Bluetooth over to my left ear, that I can hear. So, it was quite emotional one time when I came out of Boots and I had my daughter on my right-hand side and she spoke and I burst into tears and said, “My god, [name of daughter] I haven’t heard you on that side for years,” so that was quite a moving moment.
So no, the hearing’s gone, it’s never going to come back. I think they could probably do like a, something into the skull? Is it a cochlear implant? But then you’ve got to watch – I like swimming? So, you know, swimming, showers, it would just open up to infection. So, I said I’d rather, I looked into it myself and thought, “No, I’d rather not,” because when I do go on holiday, I’m always in the water, you know? I love the sea, sea salt. So, I thought, “No, I’ll just, you know, deal away with hearing aids.” And most of the time I wear them. I mean, just now I’ve got it – just one ear, my good ear, and again connected through Bluetooth. So that’s why I’m hearing you so well at the moment, but this ear’s gone. And it’s never going to come back.
And I think it’s very frustrating, I think, for people, is losing the hearing, because you almost, sort of, you know, take yourself out of social situations. I’m not always aware what’s happening in the news and that, the television might be on but I’m not picking up the same sounds as everybody else. A lot of the time I have to watch my own stuff on a screen with a you know, a hearing device in. So yeah, yeah. And even sort of in the family, my [daughter] will go, “Mum, did you hear me?” you know, people say “Did you hear that?” when we’re trying to work together, so it does impact you. But you know, at one point my hearing was the least of my problems, it was really quite low down my list of things that were wrong [laughs]. But as I get well, I think, “Oh, I’ll investigate it again,” you know, maybe five years later I’ll think, “Okay, I’m well just now, let’s go and see if anything else new has happened,” so. At the moment, no, I think I’m dealing as best as I can with it.
Isabella was “surprised” by how much nerve damage vasculitis caused in her arms and legs.
Isabella was “surprised” by how much nerve damage vasculitis caused in her arms and legs.
I will always have nerve damage to my arms and feet, I think. They did say to me that, when I got the nerve conduction tests, that it might heal completely, but I was surprised at how much damage there was in my arms and legs. At that, when I got these tests done, I think I had been on the steroids probably maybe a week or something, and I actually thought that my left leg was perfectly all right then, but they said, “Oh, there’s damage to your left, you know, your left side,” and maybe it was masked a bit by the steroid, I’m not sure.
But it was quite a bit of damage, and they said it might, you know, with time, that it would completely heal, but that really, that not to expect it. I think what he was really saying is, “Don’t expect it.” [laughs] I think that’s really what, and within, if it’s going to completely disappear, the damage, you know, this feeling, I think it would disappear, you know, within two years, so I think I’m probably going to have this forevermore.
I don’t know, it, I find that I can do most things anyway now. I can do nearly everything now, and I’ve got the feeling in my arms, and you know, the pain and the, the feeling and - but it doesn’t actually stop me doing things. So, it’s there, and I think I’ve got so used to it, it’s something I live with. And I think I’ll probably always have to live with it. It’s just yeah.
Systemic vasculitis and surgical treatments
Charlie’s vasculitis affected his airway. He had throat surgeries and a tracheostomy to help him breathe.
Charlie’s vasculitis affected his airway. He had throat surgeries and a tracheostomy to help him breathe.
And it didn’t feel quite right, so I went back to the doctor’s, and we did some tests, and then found that there were kind of two new sides of vasculitis that were - quote - more rare, that I’d started picking up for some reason, but hadn’t started before. One of them was a rare one which is inflammation of the pituitary gland, and what that impact has is kind of inducing diabetes insipidus, which means that you get very, very thirsty and you need to go to the bathroom much more. So that one was identified and that’s quite a high-risk one because the damage on the brain can be quite substantial from that.
And then the second one was that, after we did different tests and did a lot of work with ENT, we found that I’d had something called a subglottic stenosis, which is essentially inflammation, the thickening of tissue in the windpipe, just below the larynx. And what that meant was that that was getting much larger and stopping my ability to breathe.
So, with these, both these things, we suddenly had to make and kind of take quite serious action at that point. So, I had to immediately be put on cyclophosphamide and have these treatments every, every two weeks and in addition to that, I had to have numerous surgeries on my throat to be able to maintain the airway. And then this continued for a number of months, but it got to the stage that - because the surgeries were so ineffective and would only keep the airways open for three to four weeks - at that point it got, it kind of got so urgent that I ended up having a tracheostomy, as you can see now. And that was a very major surgery and I had to be in hospital for a long time at that point.
But even though it was incredibly challenging and required feeding tubes and numerous other kind of very difficult things within the hospital, as you kind of don’t realise how many things you lose from kind of having surgical work done on your throat, after that I was able to breathe easily for the first time in about six months, which was, in itself, an amazing thing. Which, which was really good.
Sharon is “doing just grand” with a kidney transplant, but it was an emotional process for all the family.
Sharon is “doing just grand” with a kidney transplant, but it was an emotional process for all the family.
We got to talking about transplants and things because the vasculitis stayed in remission, which was fabulous. So that meant that I was then a candidate for a transplant, and they do this paired pooling for donations, that’s couples can go forward. You don’t have to be a couple; could be brother, sister - friends, whatever, but you go into a database and if a couple are looking for a match with somebody else, so the way ours worked was, David volunteered to donate a kidney to somebody, and there would be somebody somewhere else in the UK that would donate to me. So, we signed up for that. Every three months they would run the database to see if you got a match. Nothing was happening. So, we did that for over a year, but we never got a match, so. But we stayed on the database.
But by that point, my mum decided that she would donate a kidney to me. She’d previously ruled herself out, she thought she was too old, but she was fit and healthy, passed all the tests, all the screening, because there’s, it’s very intrusive to make sure that you’re fit enough to donate a kidney. So, we went through, did all that, she was a perfect match, which is not always the case with your parents, but she was, so that was fab. So, we got the go-ahead for a transplant. Yeah.
It was just, like, the excitement levels, you know, this is going to be good. Obviously, there were risks, but, okay, we’ll go for it. So we went to the hospital, mum and I, they took her down for surgery and when they tried to remove the kidney, they found a tumour, a gland? On her adrenal, adrenal gland, so it was too risky to remove her kidney, so she had to come back up to ward and the transplant was, was cancelled. We were all devastated, obviously, and the focus was then on mum. Did she have a health issue? What, what had they discovered? So that all went under investigation, but she’s grand, [smiles] she’s good. But it took a wee while to suss all that out.
The consultants then spoke to me about possibly a deceased donor would be a good option, considering where we’d got to, so one night we got a phone call at three or four in the morning to say that there was a kidney. We went through, we waited, they decided after looking at the kidney a bit closer that they thought there possibly could be a cancer contamination, so they didn’t want to, to give me that one. Again, we’re devastated and come home.
A month later, we get another phone call, we go back to hospital, this one’s looking fabulous. Yeah, there’s been two kidneys, the surgeon’s already removed one to a patient in another room, it’s working perfectly, “You’ll be next, go down in two hours.” So, I go down to surgery, go in to get your, you know, put to sleep with the anaesthetic, and they decide that there is actually a problem with that kidney, so. It was cancelled at the very last second. We’re back up to the ward, home again, more devastation. The emotions are just everywhere for everyone.
We then get back to – well, a month later, they do the paired pooling match, David comes home from work, and we’re all sitting around the dinner table, and he announces that he’s had a phone call from the transplant coordinator to say that they have found us a match. At which point I am furious. I just do not have the energy to go through that again, which is not the reaction that [laughs], that I thought I would have. But. But we went. We did it. David donated his kidney. It went off in an ambulance down the M6 somewhere, mine was on route to me, and that was the 22nd, 21st of February 2017. And I’m doing just grand. [smiles and nods]
Dawn’s surgeon did “an amazing job” repairing her nose after it was damaged by vasculitis. At first, she was “terrified” to blow it.
Dawn’s surgeon did “an amazing job” repairing her nose after it was damaged by vasculitis. At first, she was “terrified” to blow it.
There are a few people that I’ve spoken to that have saddle nose deformity like mine, and there’s one very famous lady who has, she has a nose prosthesis is it? Where she actually takes her nose off. It damaged literally took away the whole nose, she just puts her nose on and takes it off.
But I’ve never seen anyone face to face who’s had saddle nose deformity like mine. My nose is now beginning to collapse again, and that’s not due to disease activity that’s just, you know, it just will, they can’t hold it there forever, it will collapse but obviously they won’t do any work on the nose until it’s absolutely necessary. They can only do so much; they can’t keep on repairing it.
But sometimes, like yesterday I looked in a photo and I said to my husband, “My nose is collapsing again,” and he said, “Yeah,” he said, “It’s going back.” It depends on how you look at the photos, you know, if I did a side shot [turns side profile] you know, you can, you can see it, but you know, people are so used to seeing my nose as it now. But it was, the operation that took place, you know, the surgeon did an amazing job with the cartilage from my ear to straighten the bridge of my nose and improve the breathing through one of the nostrils.
You said about doing the sinus washouts, that sounds horrible, what does, [laughs] what does it involve?
Oh, it was, oh, gosh it was, so I have as you may know, I have a bottle called NeilMed, I think it is, which I have to pour sachets into, and yeah, I have to hold my nose and inhale it and then flush everything that comes out, so yeah, it’s not very pleasant and can be quite embarrassing, you know, depending on where you are and things and it’s not something that can be done quietly.
But yeah, without it I’d really suffer if I couldn’t clear my nose from the horrible things that it contains, I’d find it hard to breathe and sleep at night. I think people use different things, people use Vaseline and things and salt or, you know, other remedies that they use to decongest their nose. But no, it’s not the most pleasant of things to use.
And I remember when I had my nose done and it was all impacted with, you know, everything and after that I was really, really scared to blow my nose in case I damaged everything that had been done, I was terrified, but they said, “No, it was fine.” Oh, my god, how am I going to blow my nose with this, this work that’s been done? [laughs].
Systemic vasculitis and other long-term health conditions
Vasculitis and its medication “triggered” Salma’s fibromyalgia, blood pressure problems and steroid-induced diabetes.
Vasculitis and its medication “triggered” Salma’s fibromyalgia, blood pressure problems and steroid-induced diabetes.
So, and I also have fibromyalgia, which developed in, over the years, but was diagnosed in 2007. Fibromyalgia, at that time the doctor asked me do I want any more medication for it and I said “No,” but then a year later I was re-referred to them and they then said to me, “It would be better for you if you take medication for the fibromyalgia,” because, I was in, at this, by this time I was in a lot of pain again all around the, well, all my joints and muscles would hurt and I was finding it very difficult again. And obviously with blood tests my creatinine levels and the vasculitis itself, were not too bad, they were, they might’ve been elevated a bit but not so much.
So, then my GP, I went to see my GP and she also did the same blood test, sorry, blood pressures, heart rate, oh, that’s why I’m seeing cardiology because of my heart rate was getting quite high as well at that time. Every time, my blood pressure was high, that would be high as well.
Everything that I have now has been triggered by the vasculitis in one way or the other because I, the first seven years of my working life - and I started working when I was 17 - I was, I never, ever had a sick day off work, ever. So I, obviously after that I might have had the odd few days in a year but nothing compared to what, you know, what’s happened now with the vasculitis, and I think most of it is related or started after the vasculitis, because even like the blood pressure, I didn’t used to have that problem, and because of the medication I was taking for the vasculitis that then gave me different side effects like the blood pressure and as I said, the steroid induced diabetes, and even the [fibromyalgia], all these I think comes down to, the vasculitis.
Grant had an operation to fix a slow urine flow. He is unsure if this is linked to his vasculitis.
Grant had an operation to fix a slow urine flow. He is unsure if this is linked to his vasculitis.
I should note as well, I’m speaking about involvement, sorry, involvement but obviously down below - again, this isn’t directly linked, or so we don’t think it was - just I forgot to say that at the turn of the year, I actually had a, a catheter fitted due to a urine problem, but it was more to do with a stricture in the urethra, if you, obviously, the urine tube, if you like.
But again, I don’t think they were, they couldn’t confirm or deny if it was directly linked with that because, again, for a good few years, I’ve had a slow flow of urine. For some reason, and again, I thought it was normal, but it came to a point where it was, nothing was coming out, and actually I had to get a catheter. But that’s resolved now – sorry, I actually forgot about mentioning that, so I’ve mentioned it now. But, again, they don’t know if it’s directly – they said it could be or it might not be, you know what I mean? But it’s been resolved, I’ve had an operation to kind of, kind of open up the tubing or cleaned it out, or whatever it was, so that’s kind of resolved as well. But that was just, but it wasn’t anything to do with like the liver or the kidney, it was nothing like that, it was more just a stricture. So it was, it wasn’t as bad. So, I don’t think it was quite related, but I just thought I’d mention that as well, in case it’s any relevance.
Copyright © 2024 University of Oxford. All rights reserved.


